AbstractDermatofibrosarcoma protuberans (DFSP) is a rare low-grade soft tissue sarcoma and the breast is less commonly affected than the torso. DFSP can be misdiagnosed as neurofibroma, desmoid tumor, malignant melanoma, or Kaposi sarcoma. A variant of DFSP originates from the subcutaneous layer and is called subcutaneous variant dermatofibrosarcoma protuberans (SC-DFSP). It can be easily confused with breast phyllodes tumor, myofibroblastoma, myoepithelioma, or advanced breast cancer, such as fibromatosis-like metastatic carcinoma. Following punch biopsy, the treatment of choice for breast DFSP is complete excision with negative margins ≥ 2 cm. We present a case of breast SC-DFSP with nipple areolar complex invasion.
INTRODUCTIONDermatofibrosarcoma protuberans (DFSP) is an uncommon low-grade, infiltrative skin sarcoma that arises from dermal fibroblasts. DFSP accounts for 6% of all soft tissue sarcomas and its annual incidence is approximately 0.8–5 cases per million [1]. DFSP commonly presents on the torso and less commonly on the proximal extremities (arms, legs, and neck) and breast. The incidence of breast DSFP is not well-evaluated; however, Llombart et al. [2] reported that the incidence of primary breast sarcoma is approximately 0.0006% of all breast malignancies at their institution. DSFP generally presents as a slow-growing, asymptomatic, reddish-brown mass or patch on the skin with infiltration into the dermis; therefore, it can be confused with dermatofibroma, fibrosarcoma, neurofibroma, leiomyoma, desmoid tumors, malignant melanoma, Kaposi sarcoma, and sarcoidosis [1]. Rarely, DFSP arises from the subcutaneous fat with or without dermal involvement, which is termed subcutaneous variant (SC)-DFSP. SC-DFSP appears as an asymptomatic subcutaneous mass without any changes over the skin and is commonly confused with a lipoma or sebaceous cyst [3]. DSFP is rare and SC-DSFP is rarer. Particularly, SC-DSFP of the breast is an uncommon disease with less than 10 cases reported. SC-DSFP of the breast can be misdiagnosed as fibroadenoma, phyllodes tumor, or advanced breast cancer because it looks like a protruding mass without any cutaneous changes; therefore, it is a clinically important entity. Punch, incisional, or core biopsy are recommended in establishing a diagnosis of DFSP. DFSP is a slow-growing tumor with a low malignant potential; however, it can infiltrate locally and, hence, recur frequently. The treatment of choice for DFSP is complete resection with negative margins ≥ 2 cm [2]. Here, we report an extremely rare case of breast SC-DFSP with no cutaneous changes, which was treated successfully by central lumpectomy.
CASE REPORTA 52-year-old female presented to the dermatology department with complaints of a palpable breast mass for 2 years. She was diagnosed with breast adenosis following the excision of a left breast mass 8 years ago. On physical examination, an asymptomatic subcutaneous mass was noted in the left periareolar area (Figure 1A, B). Breast ultrasonography revealed a 2.6× 0.8 cm, oval, well-marginated hypoechoic mass in the subcutaneous layer of the left upper outer periareolar area (Figure 2A). Mammography revealed an approximately 2.6 cm oval mass in the subcutaneous layer of the left upper outer periareolar breast tissue (Figure 2B). A core needle biopsy revealed an atypical spindle cell tumor; however, dermatofibrosarcoma could not be ruled out and the patient was referred to endocrine surgery. Magnetic resonance imaging revealed a 2.0 ×1.3 cm, oval, well-circumscribed, homogenous hyperechoic mass in the subcutaneous layer of the left upper periareolar breast (Figure 2C, D). The surgical plan was to perform left breast wide excision with at least 2 cm margins (Figure 3). The mass was near the nipple-areolar complex; therefore, central lumpectomy was performed including the nipple-areolar complex and parenchyma. On frozen section and permanent biopsies, the margins of the skin and parenchyma were negative, and the length of the margin and mass was approximately 2.2 cm.
Microscopically, the tumor was located near the nipple-areolar complex with invasion (Figure 4A). The tumor extended into the dermis and subcutaneous tissue. The tumor was composed of a uniform population of slender spindle cells arranged in a distinct storiform pattern (Figure 4B). No mitosis and necrosis were noted. In the peripheral regions, the spindle cells extended into the subcutaneous fat with a honeycomb-like appearance (Figure 4C). Immunohistochemically, the tumor cells were positive for CD34, but negative for cytokeratin, actin, S-100 protein, and estrogen receptor (Figure 4D). Consequently, the mass was diagnosed as DFSP.
Three months after the surgery, the breast incision site had healed well and there were no significant signs of recurrence. During follow-up, breast ultrasonography, chest computed tomography (CT), and abdominal and pelvis CT after 16 months demonstrated no detectable recurrence. Our Institutional Review Board (IRB No. CNUHH-2022-136) approved this study and waived the requirement for obtaining informed consent .
DISCUSSIONDFSP is a rare slowly growing soft tissue sarcoma that usually arises from the dermis in middle-aged adults. Darier and Ferrand [4] described it as progressive recurrent dermatofibrosarcoma and Hoffmann [5] termed it as dermatofibrosarcoma in 1925. DFSP commonly occurs on the torso and proximal extremities and rarely on the breast. Early-stage DFSP appears as a brown-red, mobile, superficial dermis-infiltrating nodule surrounded by hemangiectasis, which is similar to keloids and dermatofibromas. As it grows, the tumor looks like a blue-reddish protruding multinodular mass that spreads into the underlying subcutaneous tissue [3]. DFSP rarely occurs within the subcutaneous tissue; when it does, it is called the SC-DFSP or deep DSFP. SC-DFSP was described by Enzinger and Weiss and illustrated by Diaz-cascajo et al. [6] as an exceptional case of DFSP confined to the subcutaneous tissue. Approximately 30 cases of SC-DSFP have been reported in the literature [3]; of them, fewer than 10 cases are of breast SC-DSFP. Not all lesions appear exclusively in the subcutaneous tissues; some partially extend into the dermis. There were no significant differences in age, sex, size, or prior trauma history between patients with SC-DSFP and those with conventional cutaneous DSFP [3]. Furthermore, there were no significant differences in the clinical and histological as well as immunohistochemical features between SC-DSFP and conventional cutaneous DSFP except for the deeper location of the tumor [3,6]. On radiological evaluation, such as mammography, ultrasonography, or breast magnetic resonance imaging (MRI), SC-DFSP usually appears as a mass-like lesion located in the subcutaneous tissue. A diagnosis of DFSP should be considered when ultrasonography reveals an oval-shaped mass in the subcutaneous tissue, which is in contact with the skin and has a focal lobulated margin with hypoechogenicity or an irregular margin with mixed echogenicity [6]. Consequently, DFSP of the breast can be misdiagnosed as fibroadenoma, phyllodes tumor or advanced breast cancer either on physical examination or imaging. When a hypoechoic mass is observed on breast ultrasonography in the superficial layer with fat around the mass, DFSP can be suspected.
The standard for the diagnosis of breast DFSP is a biopsy, which can be punch, incisional, or core biopsy and must include the deep subcutaneous layer. On histopathological examination, DFSP is a tumor with spindle cells in a storiform pattern, elongated nuclei, minimal atypia, low mitotic count, and subcutaneous infiltration [7]. Tumor cells in DFSP spread along the fat tissue in a honeycomb pattern. On immunohistochemistry, CD34 is markedly positive and S-100 protein, smooth muscle actin, cytokeratin, and desmin are negative [8]. Histologically, the characteristics of SC-DFSP are hard to distinguish from those of conventional DFSP, such as storiform proliferation of spindle cells, infiltration of adipose tissue in a honeycomb pattern, and CD34 positivity on immunohistochemistry [9]. Differential diagnosis with phyllodes tumor is required which shows spindle cells present with biphasic pattern [10].
It is important to differentiate SC-DSFP from DSFP; however, from a breast surgeon’s perspective, it is also important to differentiate it from other advanced breast cancers and benign breast diseases. The differential diagnosis of conventional DSFP or SC-DSFP includes phyllodes tumor, fibroadenoma (most common), and other breast diseases, such as metaplastic carcinoma and fibromatosis [10]. Fibrosarcoma is usually subcutaneous; therefore, it is hard to distinguish it from SC-DSFP [6]. Platelet-derived growth factor (PDGF) gene rearrangement is a powerful test that can help differentiate DSFP from other breast diseases that pathologically involve spindle cell lesions. PDGF gene rearrangement testing is performed by fluorescence in situ hybridization testing on formalin fixed paraffin-embedded specimens. PDFG gene rearrangement testing was not performed in this case, but presence of the t(17;22) (q22;q13) translocation confirmed DSFP in previous study.
Breast ultrasonography can be useful to differentiate DSFP from malignant breast cancer that DSFP mass located at the dermis or subcutaneous layer with increased fat echogenicity around the mass [11]. Breast MRI can be helpful in pre-operative evaluation to check the tumor extent after histopathological confirmation. On breast MRI, DFSP demonstrates a high T2, low T1 signal. DFSP can metastasize to the lungs and lymph nodes with 14.5% of risk, so evaluation before surgery through comprehensive imaging modality is necessary which includes routine CT or MRI [7].
Due to the locally aggressive, infiltrative, and radiotherapy and chemotherapy-resistant characteristics of DFSP, the treatment of choice for localized DFSP is complete surgical excision with negative margins. The local recurrence rate of DFSP within 3 years of local excision is up to 50%; therefore, sufficient clear margins should be secured. National Comprehensive Cancer Network guidelines recommend Moh’s microscopic surgery (MMS) or other forms of peripheral and deep en face margin assessment (PDEMA); however, if MMS or other forms of PDEMA are unavailable, wide excision can be considered [12]. For SC-DFSP, the treatment of choice is the same as that for conventional DFSP. According to a retrospective series of 18 patients by Llombart et al. [3], SC-DFSP needed more MMS stage than DSFP. All margins are assessed using histopathological examination. When positive margins are noted on frozen section histopathology, re-resection should be performed until negative margins are verified. Adjuvant radiation is used in cases of persistent positive margins, gross disease, or unresectable DFSP. PDGF gene rearrangement results in the formation of a COL1A1-PDGFB chimeric gene, and mature PDGFB collagen-producing cells induce autocrine growth stimulation, and this mechanism can be used to formulate targeted therapy with tyrosine kinase inhibitors, such as imatinib mesylate [13,14]. If the size of the tumor is too big to achieve negative margins, neoadjuvant imatinib can be considered. McGee et al. [8] reported a case of neoadjuvant imatinib therapy in order to perform breast-conserving surgery according to the wishes of the patient; they reported a 40% reduction in tumor size.
Currently, the recommended adequate margin width for DFSP resection is approximately 2–3 cm to minimize local recurrence. When a 1-cm margin is used around the tumor, residual tumor cells can be found in more than 70% of patients. The local recurrence rate reduces to less than 1% when the resected margin is extended to approximately 2 cm [7]. In our patient, DFSP of the breast near the nipple-areolar-complex was completely resected using 2 cm margins. Approximately 7 months following the central lumpectomy, there were no signs of recurrence.
In conclusion, SC-DFSP of the breast is located in the subcutaneous layer with no symptoms; therefore, it is hard to distinguish it from benign breast lesions or invasive breast cancer using only physical examination. It is important to ascertain the location of the mass using imaging studies, such as breast ultrasonography and core needle biopsy. Treatment of SC-DFSP is complete excision of the mass, which may be accomplished using MMS, PDEMA, or wide excision with 2 cm margins.
Figure 1.Preoperative images of the case. (A, B) A 2.6 cm sized protruding subcutaneous mass at left upper periareolar area. 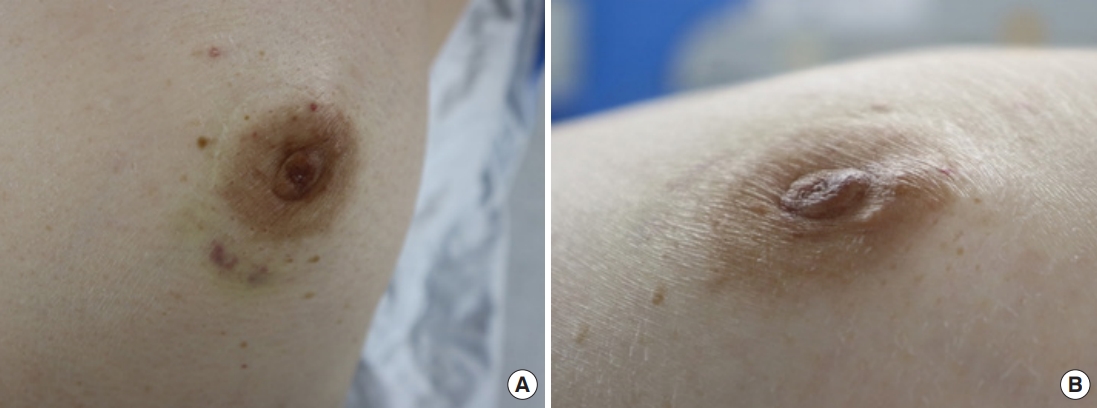
Figure 2.Preoperative radiologic examinations. (A) Ultrasonography. A 2.6×0.8 cm sized oval-shaped hypoechoic mass at subcutaneous layer of left periareolar breast. (B) Mammography. Oval mass in subcutaneous layer of left upper outer periareolar breast. (C, D) Breast Magnetic Resononce Imaging. A oval homagenous enhancing mass at left upper periareolar subcutaneous layer involving skin layer. 
Figure 3.Before central lumpectomy, excision line was drawn in order to minimize local recurrence, resting skin tension and maximize cosmetic outcome (A, B). (C) Breast tissue removed, along with skin. 
Figure 4.Dermatofibrosarcoma protuberans. (A) Low magnification view showing a tumor located the near the nipple-areolar complex (H&E, ×1). (B) Spindle cells arranged in storiform pattern (H&E, ×200). (C) Spread of spindle cells into subcutaneous fat with honeycomb-like appearance (H&E, ×100). (D) Diffuse CD34 positive immunoreactivity (H&E, ×100). 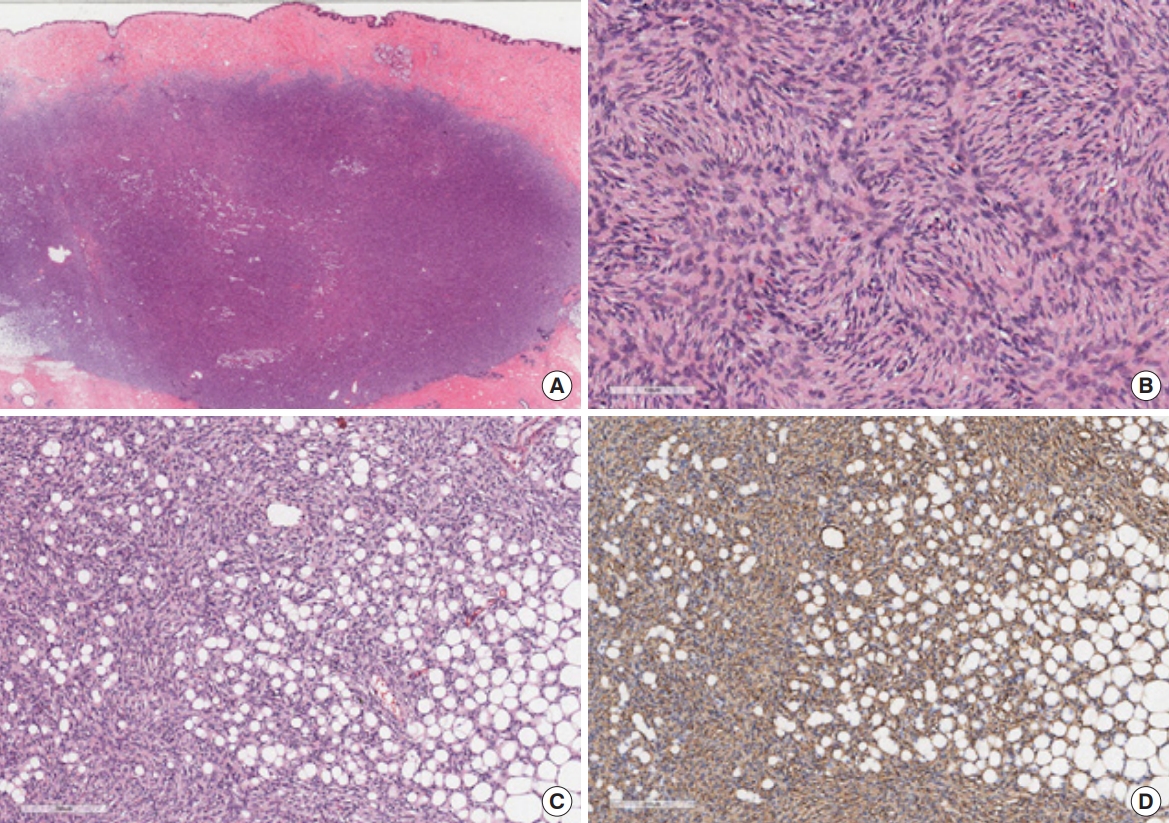
REFERENCES1. Ferreira ALS, Souza JA, Gibbons IL, Lellis RF, Oliveira VS, de Sousa, et al. Clinical and imaging features of dermatofibrosarcoma protuberans in the breast. Breast J 2021;27:92-4.
2. Llombart B, Serra-Guillén C, Monteagudo C, López Guerrero JA, Sanmartin O. Dermatofibrosarcoma protuberans: a comprehensive review and update on diagnosis and management. Semin Diagn Pathol 2013;30:13-28.
3. Llombart B, Serra-Guillen C, Rubio L, Nagore E, Requena C, Traves V, et al. Subcutaneous dermatofibrosarcoma protuberans, a rare subtype with predilection for the head: a retrospective series of 18 cases. J Am Acad Dermatol 2017;77:503-11.e1.
4. Darier S, Ferrand M. Recurrent or progressive dermatofibromas and fibrosarcoma of the skin. Ann Dermatol Venereol 1924;5:545-62.
5. Hoffmann E. Regarding the knollentrichencle fibrosarcoma of the skin (dermatofibrosarcoma protuberans) (In German). Dermatol 1925;43:1-28.
6. Diaz-cascajo C, Weyers W, Rey-lopez A, Borghi S. Deep dermatofibrosarcoma protuberans: a subcutaneous variant. Histopathology 1998;32:552-5.
8. McGee MW, Boukhar SA, Monga V, Weigel R, Phadke SD. Dermatofibrosarcoma protuberans-the use of neoadjuvant imatinib for treatment of an uncommon breast malignancy: a case report. J Med Case Rep 2019;13:374.
9. Bague S, Folpe A. Dermatofibrosarcoma protuberans presenting as a subcutaneous mass: a clinicopathological study of 15 cases with exclusive or near-exclusive subcutaneous involvement. Am J Dermatopathol 2008;30:327-32.
10. Wang Y, Wang Y, Chen R, Tang Z, Liu S. A rare malignant disease, dermatofibrosarcoma protuberans of the breast: a retrospective analysis and review of literature. Biomed Res Int 2020;2020:8852182.
11. Noh JH, Min JW, Myung NH, Kim YM. Ultrasonographic and pathologic findings of dermatofibrosarcoma protuberans of the breast: a case report. J Korean Soc Radiol 2018;78:349-52.
12. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology for Guideline Dermatofibrosarcoma Protuberens Version 2. 2022.
13. Patel KU, Szabo SS, Hernandez VS, Prieto VG, Abruzzo LV, Lazar AJF, et al. Dermatofibrosarcoma protuberans COL1A1-PDGFB fusion is identified in virtually all dermatofibrosarcoma protuberans cases when investigated by newly developed multiplex reverse transcription polymerase chain reaction and fluorescence in situ hybridization assays. Hum Pathol 2008;39:184-93.
|
|
||||||||||||||||||||||||||||||||||