INTRODUCTION
Breast cancer is one of the most common malignancies among Korean women after thyroid cancer. Korea has a low breast cancer incidence rate (43.8 per 100,000 women-years in 2009) [1], which is increasing at a rapid rate. The crude incidence rate of breast cancer among Korean women in 2015, including carcinoma in situ, was 88.1 per 100,000, a significant increase from 26.3 in 2000 [2]. In Korea, the five-year survival rate is 91.2% (89.2% in the US and 89.1% in Japan), showing an increase from 83.2% (1996–2000) to 88.5% (2001–2005) [3]. The incidence and death rates of breast cancer differ slightly among countries. Worldwide, from 1980 to 2010, the number of breast cancer cases has been steadily increasing, and the incidence of breast cancer is increasing at an annual rate of 3.1%, and mortality from breast cancer is increasing at an annual rate of 1.8%. Breast cancer is the leading cause of cancer-related deaths with an estimated 1.7 million cases and 521,900 deaths in 2012. Breast cancer accounts for 25% of all cancer cases and 15% of all cancer-related deaths among women [4].
In future, screening that includes mammography and ultrasonography can help reduce the incidence of advanced cancer and breast cancer mortality owing to early detection of breast cancer [5]. Many randomized controlled trials (RCTs) have shown that routine screening mammography for women aged over 40 years can help early detection of breast cancer and decrease breast cancer mortality by over 30% [6]. The effect of screening in reducing breast cancer mortality persists with long-term follow-up. The effect is age-dependent: the highest effect is seen in women aged 55–69 years and lowest, in women aged 50–54 years, at randomization [7].
Hospital volume can be categorized into three levels : low volume (<148 cases/year), moderate volume (148–298 cases/year), and high volume (>298 cases/year) [8]. Our center is a low-volume center. The purpose of this study was to analyze breast cancer treatment outcomes in a low-volume center.
METHODS
This study was approved by Institutional Review Board at the chosun university hospital (IRB No. 2019-08-024-001). Data were collected from the records of patients who were newly diagnosed with primary breast cancer during the period of January 1998 to December 2013 at Chosun university hospital, South Korea. Clinical and pathological data were extracted from electric medical records. The following parameters were extracted: surgical method, pathological stage (American Joint Committee on Cancer [AJCC], eighth edition), tumor, node, metastasis (TNM) stage, histological categorization, hormone receptor status, and human epidermal growth factor receptor 2 (HER2) positivity. Survival analysis was performed for disease-free survival (DFS) and overall survival (OS) by the Kaplan-Meier method based on anatomic stage. The level of significance was set at 5% for all statistical tests. All statistical analyses were performed using SPSS21.0 (SPSS Inc., Chicago, USA)
RESULTS
Number, sex, and age distribution of patients
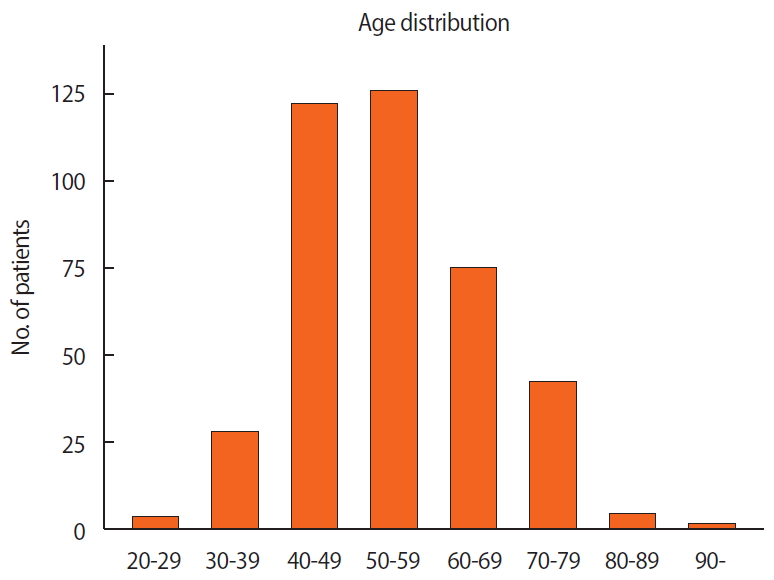
In our center, there were 401 cases of newly diagnosed breast cancer (Table 1), with 5 (1.2%) male breast cancer patients. The median age was 52 years. The largest number of newly diagnosed patients was in the 50–59 years age group (126 cases, 31.4%), followed by the 40–49 years age group (122 cases, 30.4%) (Figure 1).
Surgical approach and staging
The types of surgical approaches adopted at our center from 1998 to 2013 were breast-conserving surgery (BCS) (153, 38.2%), modified radical mastectomy (MRM) (243, 60.6%), wide excision (4, 1.0%), and others (1, 0.2%).
In all, 117 patients (29.2%) were in stage I, 176 (43.9%) in stage II, and 78 (19.4%) in stage III of the disease. Stage IIa was the most common disease stage, with 120 cases (32.2%), followed by stage I (29.2%) (Table 2).
Pathological features and biomarkers
Among the 401 patients, invasive ductal carcinoma was the most common diagnosis, with 346 cases (86.3%), followed by ductal carcinoma in situ (DCIS), with 35 cases (8.7%). According to histological type, there were 43 cases (DCIS: 35, LCIS: 8) of non-invasive carcinoma, 350 cases (87.3%) of invasive carcinoma, 2 cases (0.5%) of Paget’s disease, 1 case (0.2%) of malignant phyllodes tumor, 3 cases (0.7 %) of sarcoma, and 2 cases (0.5 %) of other types (Table 2).
Estrogen-receptor (ER)- and progesterone-receptor (PR)-positive cases accounted for 53.4% of all cases. Tumors types that were positive for both hormone receptors were observed in 144 cases (35.9%) and those that were negative for both hormone receptors, in 129 cases (32.2%) (Table 2).
Five-year survival and overall survival
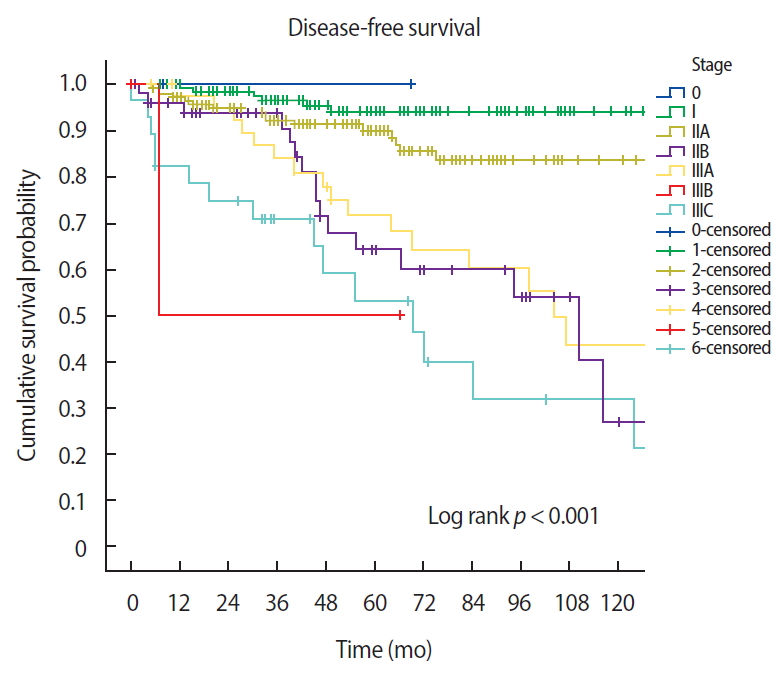
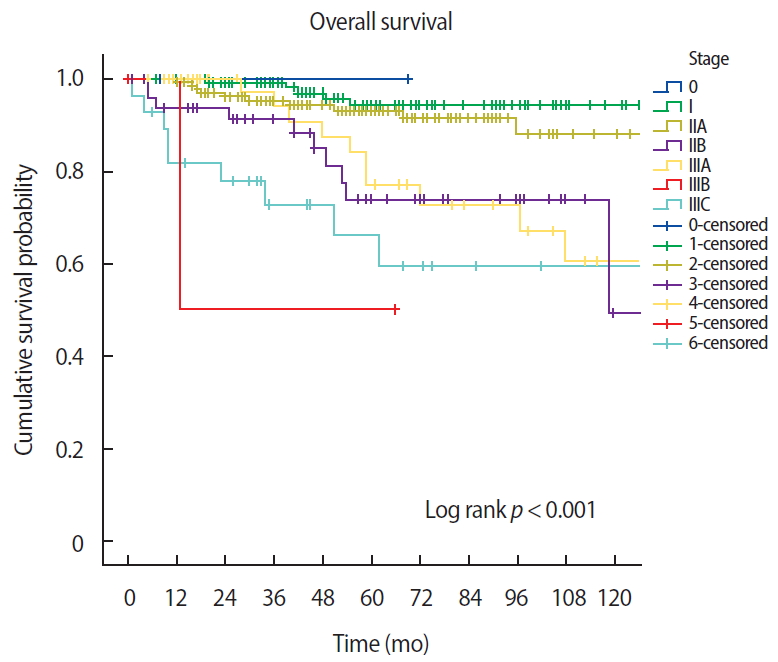
The five-year DFS rates were 100% (stage 0), 95.4% (stage I), 91.4% (stage IIa), 75% (stage IIb), 78% (stage IIIa), 50% (stage IIIb), and 59.2% (stage IIIc) (Log rank p<0.001) (Figure 2). The OS rates were 100% (stage 0), 96.2% (stage I), 94.3% (stage IIa), 85.4% (stage IIb), 84.8% (stage IIIa), 50% (stage IIIb), and 55.5% (stage IIIc) (Log rank p<0.001) (Figure 3).
DISCUSSION
The number of newly diagnosed breast cancer patients in South Korea has been increasing [9]. Although the reasons for the increasing trend are not completely understood, it likely reflects birth-cohort effects, changes in reproductive factors (early menarche, late childbearing, and having fewer children), diet (i.e., consumption of high-calorie foods), obesity, and the introduction of screening programs [10]. In Korea, the median age of newly diagnosed patients in 2010 was 49 years, which was slightly higher than that in the past, but is more than 10 years lower than that in the US [11]. The median age reported in our hospital is similar to that in all of Korea.
Breast cancer in men is being diagnosed at early stages. The percentage of breast cancer cases diagnosed at stage 0 or I has consistently increased from 7.0% to 31.1% in 2002 and from 14.8% (111.4% increase; R2 = 0.847, p<0.001) to 43.3% (25.8% increase; R2 = 0.894, p<0.001) in 2015 [12]. In breast cancer RCTs, there was a decrease in the risk of being diagnosed with advanced breast cancer because of mammographic screening programs [13]. The ratio of early breast cancer (stages 0 and I) cases increased from 38.1% of all breast cancer cases in 2002 to 55.7% in 2014 [14]. At our center, the percentage of cases diagnosed at stage 0 or 1 was 37.6% (147 patients) from 1998 to 2013.
In Korea, the ratio of BCS is found to surpass that of mastectomy. The proportion of patients undergoing BCS is twice that of patients undergoing mastectomy patients (67.2% vs. 32.3%) [15]. However, in recent years, the patients undergoing mastectomy has been slightly increasing [16]. At our hospital, MRM is still the most common breast cancer surgery. In recent years, the proportion of BCS has shown a steady increased.
In our hospital, there were 214 (43.4%) ER-positive or PR-positive breast cancer patients (Table 2). There has been a recent increase in the proportion of ER-positive breast cancer cases worldwide [11]. A similar trend has been observed in Korea and Japan [17]. There are some reports on the reasons behind the increase in ER-positive breast cancer [18]. Yip et al. [19] reported that ER positivity was significantly associated with early stage (I, II) and low-grade breast cancers. Ko et al. [11] examined this recent trend, noting that the incidence of ER-positive breast cancers will increase, the incidence of ER-negative breast cancers will decrease, and the overall incidence of breast cancer will remain steady.
Breast cancer is the second most common cause of death and accounts for 14% all new cancer diagnoses in women [4]. The five-year relative survival rates (%) for breast cancer in all races increased from 84% during the mid-1970s to 91% in 2005–2011 [4].
Especially, patients with ER/PR-positive breast cancer experienced significant survival gains across all stages, and the highest annual increase in survival rates was reported for women is stages III and IV of the disease [20].
In Korea, the five-year survival rate is 91.2% (89.2% in the US, 89.1% in Japan), increasing from 83.2% (1996–2000) to 88.5% (2001–2005) [11]. For each stage, the five-year OS rates were 98.3% (stage 0), 96.6% (stage I), 91.8% (stage II), 75.8% (stage III), and 34.0% (stage IV) [14].
The five-year DFS rates in our hospital were 100% (stage 0), 95.4% (stage I), 91.4% (stage IIa), 75% (stage IIb), 78% (stage IIIa), 50% (stage IIIb), and 59.2% (stage IIIc). This result corresponds to that of a previous large-scale clinical study [3]. However, the proportion of stage III cases is slightly different from that reported in the large-scale clinical study due to the small number of patients in our study.
In many studies, high-volume centers were found to be independent predictors of improved OS, and a direct inverse relationship between volume and mortality from high-risk surgical procedures for cancer has been reported [8].
Our study has a few limitations such as the small sample size. However, we have shown favorable survival outcomes despite our center being a low-volume one. Although further investigation involving collaboration between different low-volume centers is needed, patients can be treated at low-volume centers with excellent outcomes.